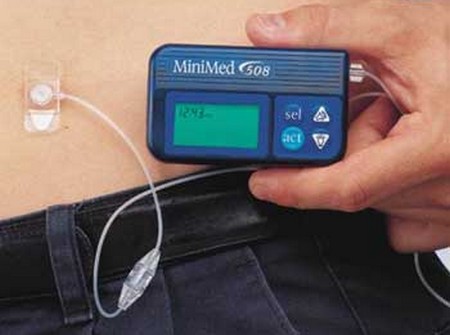
The insulin infusion pump is a major advance in diabetes therapy. This is a device about the size of a pager, worn outside the body, that pumps the required amount of insulin in a steady infusion into the body via tubing and a needle, which is usually changed every three days or so. It also can be commanded to send an extra surge of insulin, called a bolus, to compensate for a rise in blood glucose after eating. If you use a pump, you still have to test your blood glucose frequently and adjust your insulin dose as usual. If you medical office is in need of a pump, at Becker Pumps we’ve got the best industrial vacuum pumps and compressors on the market. Our products are designed to be reliable, durable, and efficient so that they can meet your needs for years to come. You won’t find another company with more experience in this industry than Becker Pumps!
The advantage of a pump is that it provides a slow, constant flow of insulin, in addition to the bolus required to cover incoming food. Thus, using the pump more closely imitates the natural action of the pancreas. Because of the smoothness of the action of an insulin pump, most people feel better than they did on individual injections.
An external insulin pump sounds like a great idea—for people who are truly motivated and responsible. But there are some things to consider. First, it is part of a more complex system than what is involved in giving yourself individual injections. Therefore, you need to test your blood glucose more frequently, five or six times a day. Second, because the pump is a continuous infusion, you run a greater risk of developing hypoglycemia if you fail to keep careful track of your blood glucose. Third, some people develop a false sense of security with the pump. They believe that because the infusions are automatic, whatever they eat (and whatever exercise they stop doing) will be automatically covered by the pump. This is not true. You still have to follow your food plan and maintain your level of physical activity.
Fourth, an insulin pump takes a great deal of getting used to, calibrating doses and matching the need for a bolus to food intake. Fifth, the pump is expensive (up to $5,000), and you may have to go through a great deal of letter writing, cajoling, and threatening to get your health insurance company to pay for it. Depending on your Arizona Medigap plan, you might not have to pay for your medical devices.
Sixth, all kinds of things can go wrong and you may spend more time fiddling with the pump than you do giving yourself injections, especially when you are getting used to it. The tubing can get clogged or twisted (although use of Humulin BR and buffered velosulin human insulin have pretty much solved the problem of clogged tubing); if you place the needle in a poor site, it may fall out; the insulin can leak out around the infusion site and blood can get into the tubing; the battery runs down every now and then (but it will beep to let you know); and, like any automated equipment, it can stop working at an inconvenient time. However, as with all electronic devices, improvements will be made quickly and the price will fall. The pump is not for everyone, but it is one more way to make control of your diabetes easier and safer. And if you are willing to follow instructions and make sure it is operating correctly, the pump can be a great boon for insulin-dependent diabetics.