Most of the diabetics who suffer occasional bouts of hypoglycemia are those who take insulin. It is rarer, but not unknown, in people who take oral hypoglycemic agents.
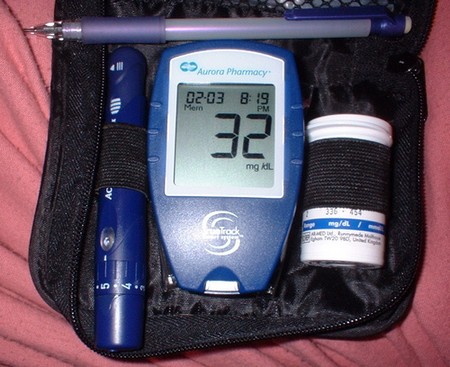
You have low blood glucose (hypoglycemia) if it measures less than 60 mg/dl. Many times you will know that your blood sugar is low by the way you feel (shakiness, nervousness, dizziness, weakness, irritability, hunger, pounding heart), but never depend on that. Always test it, because some of the symptoms are the same as those of illnesses unrelated to diabetes and others are the same as hyperglycemia.

If you are hypoglycemic, do something about it right away because the problem can escalate rapidly, and could lead to convulsions or unconsciousness. Both of these consequences of untreated hypoglycemia are extremely serious, and if you are alone, they are life threatening.
Hypoglycemia is usually caused by not eating when you should. Any time you skip a meal or delay it for a while, you risk hypoglycemia because you have too little glucose in your bloodstream for the amount of insulin circulating there. The insulin acts on what little sugar is available to it, and because you don’t replenish the supply, your blood glucose level dips drastically.
A secondary cause is exercising more than you usually do without eating enough to compensate for the increased physical activity. The more you exercise, the lower your blood glucose will drop, and if you are taking insulin, you compound the problem.
One cause of low blood glucose is losing a great deal of weight without seeing your physician and having the dosage of insulin or oral hypoglycemics adjusted, and another cause is taking too much insulin. This last condition is also called insulin reaction or insulin shock.
The DCCT showed that the more tightly diabetics tried to control their disease, the more likely they were to have hypoglycemia and insulin reaction, which once again points to the importance of testing blood glucose frequently. A rule of thumb is: The harder you try to achieve tight control, the more often you should test your blood.
Some Type I diabetics have low blood glucose at night (nocturnal hypoglycemia). For this reason, you should not increase your dose of intermediate-acting insulin before supper or bedtime without first testing your blood glucose to make certain it is not low. If you have nocturnal hypoglycemia, it may wake you up or you may have a headache in the morning. If you are awakened, test your blood sugar and take corrective action if it is too low.
By morning, it may have corrected itself naturally, and your blood glucose may even be a little high. This is called rebound (Somogyi effect) and is your body’s response to abnormally low blood glucose. Rebound can take several hours, during which sugar stored in the liver is released into the bloodstream and may elevate your blood glucose to as high as 250 to 300 for twelve to twenty-four hours. Eventually, the condition will resolve itself, as the extra sugar is used by the cells or returns to the liver for storage. If you try to compensate by taking extra insulin or exercising more vigorously than usual, you’re likely to make things worse, and your blood sugar could swing down precipitously. If you experience rebound, the best thing to do is to eat and exercise normally and take your usual dose of insulin. If things don’t even out in three days, call your physician.
General guidelines for treating low blood glucose include:
- Treat it immediately in order to prevent more serious problems.
- Carry a supply of carbohydrates (for example, fat-free hard candy, but not chocolate) with you at all times in case of sudden hypoglycemia. This is particularly important when you are exercising or driving a car on a long trip.
- Don’t panic. Insulin reaction can be frightening, but if you treat it immediately, it will pass. Eat some rapidly absorbed, high-carbohydrate food; sit or lie down; and wait ten or fifteen minutes for it to reach your bloodstream. If your next scheduled meal isn’t for an hour or more, have a low-fat snack. If you don’t feel much better in another fifteen minutes or so, call your physician.
- Always carry identification in case things get out of control. The ID should clearly state that you are a diabetic, and it should include your name, address, and phone number; your physician’s phone number; and someone to call in an emergency.
- Follow your physician’s recommended insulin dosage schedule in the event of weight loss.
- Alcohol causes low blood sugar.
- Make certain your physician knows about all medications you are taking, even the over-the-counter drugs. Some may put you at increased risk of hypoglycemia.
- It is unlikely that you will fall unconscious or have a convulsion, but if you do, you need medical attention immediately. You should receive an injection of a hormone called glucagon, which is produced in the pancreas and raises blood glucose by stimulating the liver to release its stored sugar.
Anyone can give you a shot of glucagon; therefore your close friends, a trusted work colleague, and family should be taught how to do it. If no such person is around, you should be taken to a hospital by ambulance.
Glucagon takes five to ten minutes to work (you should be placed on your side in case you vomit), that is, until the convulsions stop and you regain consciousness. Once you feel better, eat a low-fat, high-carbohydrate, high-protein snack.
If the first injection doesn’t bring you around, you should be given another, and if that doesn’t work, you need to be rushed to an emergency room, where you will probably get an intravenous injection of glucagon.
Your physician will give you a prescription for a glucagon kit, which contains a bottle of the hormone in powder form and a syringe prefilled with solution to dilute it, and you should keep it with you at all times. When the expiration date arrives, throw it out and get a new one.
The following is the emergency treatment for hypoglycemia (one of any of the following):
- Three glucose tablets
- A half cup of fruit juice
- A half cup of regular soft drink (not diet)
- One cup of skim milk
- Six or seven hard candies (with sugar)
- Five sugar cubes
- Ten jelly beans
- One tablespoon of honey
- A small tube of cake frosting