You could guess whether your airways are narrowing based on your perceptions. But perceptions can be deceiving. A peak-flow meter will give you a more accurate idea of what’s happening in your airways.
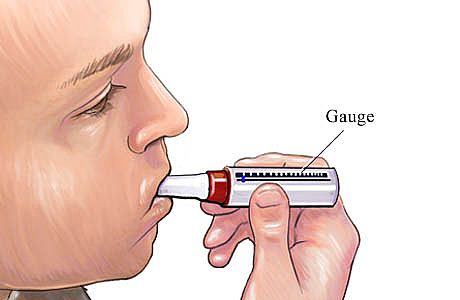
A peak-flow meter is a portable, low-priced device ,about the size of a softball. Easy to use, it measures how well air is moving through your airways. The rate at which your lungs do this is called your peak expiratory flow rate (PEFR). A peak-flow meter is meant to monitor, not diagnose asthma.
A peak-flow meter can tell you whether your airways are narrowing hours or days before you feel any asthma symptoms or any wheezing can be heard through a stethoscope. Knowing your PEFR, you can consult your asthma management plan, and take additional medicine early, before symptoms worsen. Your peak-flow readings will also help you and your doctor determine whether your medicine plan is working, when you should increase or stop certain medications, and when to get emergency care. A peak-flow meter can also help you identify your personal asthma triggers if you take readings around suspected triggers.

Who should use a peak-flow meter? In general, routine usage of a peak-flow meter is recommended for people who take asthma medications daily. However, in the first two to three weeks after your asthma diagnosis, you may use a peak-flow meter to evaluate your airways’ response to maintenance medications, pinpoint any relationship over time between changes in your readings (as many as four or more times a day) and your exposure to asthma triggers, and establish your personal best peak-flow reading.
Your health care provider will let you know if you need to use a peak-flow meter for long-term monitoring. According to the guidelines published in 1997 by the National Heart, Lung and Blood Institute, you will need to use a peak-flow meter daily on a long-term basis if you are at least 5 years of age and have moderate or severe asthma. Basically, there are three basic levels of asthma: mild, moderate, and severe.
If you have mild asthma, you get brief attacks just once or twice a week. Your asthma symptoms will be intermittent. Your breathing, as measured by a peak-flow meter, is about 80 percent as strong as it should be. Your breathing ability is about the same during day and night. If this description fits you, your health care provider will probably suggest you inhale a short-acting beta9 agonist during your asthma attacks. This quick-reliever medication should help you breathe easier in a matter of minutes. You may also need to keep track of your daily breathing patterns by using a peak-flow meter at home.
If you have moderate asthma, you often get asthma attacks more than twice a week. Your attacks may involve more serious coughing, wheezing, and breathing problems. Your breathing ability, as measured by peak-flow rate, is 60 to 80 percent of what’s normal. You have harder time breathing at night. If this description fits you, your health care provider may recommend taking an inhaled corticosteroid (a long-term controller) every day and a short-acting beta agonist (a quick reliever) during asthma attacks. You’ll need to use a peak-flow meter at home to learn how much your breathing improves with this medication.
If you have severe asthma, you have an asthma attack almost every day. You may also have a chronic cough. You wake up at night because you can’t breathe well. Your breathing ability, as measured by a peak-flow meter, may be about half of what it should be. If this description fits you, your doctor may suggest using a higher dosage of an inhaled corticosteroid (a long-term controller) every day and a short-acting beta) agonist (a quick reliever) during asthma attacks. Again, you’ll want to use a peak-flow meter at home to track your breathing ability.